Living with lumbar spinal nerve root inflammation caused by a herniated disc can feel like an uphill battle, especially when pain disrupts your sleep.
The right mattress can be a game-changer, offering relief by supporting your spine, easing pressure, and promoting restorative rest.
This comprehensive guide dives deep into the condition, the critical role of sleep posture, and the mattress qualities—firmness, materials, and support zones—that can help manage pain and improve your quality of life.
We’ll compare popular mattress types, incorporate insights from medical research, and address common concerns in a detailed FAQ, all while weaving in related terms like spinal health, back pain relief, and ergonomic sleep solutions to provide a holistic perspective.
What Is Lumbar Spinal Nerve Root Inflammation and Disc Herniation?
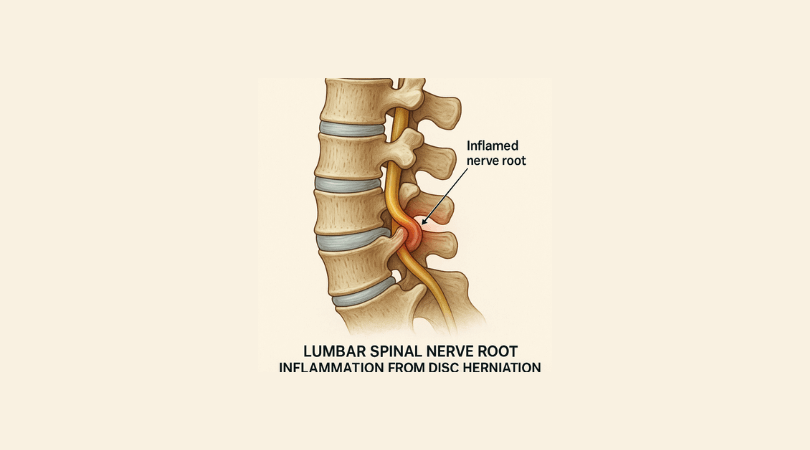
Lumbar disc herniation occurs when the soft, jelly-like core of a spinal disc (nucleus pulposus) pushes through a tear in its tough outer layer (annulus fibrosus), typically in the lower back (lumbar spine). This bulge or rupture can press against or irritate nearby nerve roots, triggering inflammation and symptoms like sharp pain, numbness, tingling, or weakness that may radiate down the legs (sciatica). The condition often stems from age-related disc degeneration, repetitive strain, or sudden injury, such as lifting heavy objects improperly.
- Prevalence and Impact: Affecting 1-3% of adults, with a higher incidence in those aged 30-50, disc herniation is a leading cause of chronic lower back pain. Sleep disturbances are common, as lying down can exacerbate nerve compression.
- Symptoms in Daily Life: Pain may intensify with sitting, bending, or poor posture, making restful sleep challenging. Nighttime discomfort can hinder recovery, as sleep is essential for reducing inflammation and healing.
- Medical Context: Treatment often includes physical therapy, anti-inflammatory medications, or, in severe cases, surgery like discectomy. A supportive mattress complements these efforts by minimizing spinal stress during sleep.
- Related Conditions: Sciatica, radiculopathy, and degenerative disc disease often accompany herniation, amplifying the need for proper sleep support.
A mattress tailored to this condition can reduce nerve irritation, align the spine, and create an environment conducive to healing, making it a cornerstone of pain management.
Why Sleep Posture Matters for Spinal Health

Sleep posture profoundly influences how your spine, discs, and nerves bear weight during rest. For those with lumbar nerve root inflammation, improper positioning can worsen pain by compressing nerves or straining the lower back. The goal is to maintain the spine’s natural curves—cervical, thoracic, and lumbar—while minimizing pressure on the herniated disc.
- Optimal Sleep Positions:
- Side Sleeping (Fetal Position): Curling slightly with knees bent opens the spaces between vertebrae, reducing nerve root pressure. A pillow between the knees keeps the pelvis and spine aligned, preventing twisting that could aggravate sciatica.
- Back Sleeping: Lying flat with a thin pillow under the knees or a rolled towel under the lower back supports the lumbar curve, evenly distributing weight and easing disc pressure. Use a low-profile head pillow to avoid forward tilt of the neck.
- Why Avoid Stomach Sleeping: This position arches the lower back, increasing disc protrusion and nerve compression. It also strains the neck, contributing to overall discomfort.
- Posture Challenges: Shifting positions during sleep is common, especially if pain disrupts rest. A mattress must adapt to these changes, providing consistent support whether you’re on your side or back.
- Role of Bedding: Pillows and mattress toppers enhance posture. For example, a contoured cervical pillow supports neck alignment, while a topper can fine-tune mattress firmness.
- LSI Keywords: Spinal alignment, ergonomic sleep, back pain relief, sciatica support, lumbar health.
A mattress that promotes neutral spinal alignment and cushions sensitive areas is essential for reducing nighttime pain and supporting long-term recovery.
Essential Mattress Qualities for Pain Relief and Comfort
Selecting a mattress for lumbar disc herniation involves balancing support, pressure relief, and durability. The right combination of firmness, materials, and design features can alleviate nerve root inflammation, reduce morning stiffness, and improve sleep quality. Below are the key qualities to prioritize, with detailed explanations to guide your choice.
- Firmness Level:
- Medium-Firm (5-7/10): Research, including a 2003 study in The Lancet, found medium-firm mattresses outperform overly soft or rigid ones for low back pain. They contour to the body’s curves while preventing excessive sinking, which can misalign the spine.
- Why It’s Effective: Soft mattresses (<4/10) allow the hips to sag, twisting the lumbar spine and worsening nerve compression. Very firm mattresses (>8/10) create pressure points at the hips and shoulders, increasing discomfort, especially for side sleepers.
- Personalization: Body weight matters—lighter individuals (<150 lbs) may prefer slightly softer medium-firm mattresses, while heavier individuals (>200 lbs) need firmer options to prevent sinking.
- Support Zones:
- Zoned Construction: Mattresses with targeted support—firmer foam or coils under the hips and lower back, softer under the shoulders—promote neutral alignment. This design is particularly beneficial for side sleepers, as it prevents the pelvis from tilting.
- Lumbar Reinforcement: Enhanced padding or denser materials in the lumbar region maintain the spine’s natural “S” curve, reducing stress on inflamed nerves.
- Benefits: Zoned support minimizes spinal curvature, which a 2017 study in Journal of Orthopedic Research linked to reduced back pain in patients with disc issues.
- Materials:
- Memory Foam: High-density memory foam (4-5 lbs/ft³) molds to the body, cradling pressure points like the hips and shoulders. It excels at distributing weight evenly, reducing stress on the lumbar spine.
- Latex: Natural or synthetic latex is responsive, offering a buoyant feel that prevents the “stuck” sensation of memory foam. It’s naturally cooling and durable, lasting 10-15 years.
- Hybrid (Innerspring + Foam/Latex): Combining pocketed coils for support with foam or latex layers for cushioning, hybrids provide breathability and adaptability, ideal for combination sleepers.
- Avoid Low-Quality Materials: Budget foam (<3 lbs/ft³) or basic innerspring mattresses with minimal padding degrade quickly, losing their ability to support spinal health.
- Cooling Features: Gel-infused foam or perforated latex dissipates heat, addressing inflammation-related warmth sensitivity.
- Pressure Relief:
- A 2-3 inch comfort layer of foam or latex cushions bony prominences, critical for side sleepers with sciatica. This reduces numbness and tingling in the legs.
- Pressure-relieving mattresses also minimize tossing and turning, which a 2019 study in Sleep Medicine associated with improved sleep quality in back pain patients.
- Edge Support:
- Reinforced edges (high-density foam or sturdy coils) make it easier to get in and out of bed, a common challenge for those with back pain. This feature also maximizes usable sleep surface for couples.
- Strong edges are especially helpful for older adults or those with mobility issues.
- Motion Isolation:
- Memory foam and latex excel at absorbing motion, ensuring that a partner’s movements don’t disrupt sleep. This is vital for light sleepers with pain-related sleep disturbances.
- Hybrids with pocketed coils also offer good motion isolation compared to traditional innerspring mattresses.
- Mattress Thickness:
- A 10-12 inch mattress provides sufficient support and comfort for most. Heavier individuals may need 12-14 inches to ensure adequate lumbar support and durability.
- Thicker comfort layers (3+ inches) enhance pressure relief but may compromise support if the base layer is too thin.
- LSI Keywords: Mattress firmness, lumbar support, pressure relief, spinal health, back pain mattress, sciatica relief.
Comparing Mattress Types: Memory Foam, Latex, and Hybrid

Each mattress type offers distinct advantages for managing lumbar nerve root inflammation. Below is an in-depth comparison to help you choose based on your sleep style, budget, and comfort preferences.
- Memory Foam:
- How It Works: Memory foam softens with body heat, conforming closely to your shape. This reduces pressure on the hips, shoulders, and lower back, ideal for side sleepers with sciatica.
- Pros:
- Superior pressure relief, minimizing nerve irritation.
- Excellent motion isolation, perfect for couples.
- Wide range of firmness options, from medium to medium-firm.
- Cons:
- Can trap heat, though gel or open-cell foam mitigates this.
- Slower response time, which may feel restrictive for combination sleepers.
- Lower-quality foam may sag within 5-7 years.
- Best For: Side sleepers, those with acute pain, or anyone prioritizing contouring comfort.
- Example: A 12-inch medium-firm memory foam mattress with a gel-infused top layer and a high-density base for lumbar support.
- Latex:
- How It Works: Latex provides a springy, responsive feel, contouring less intensely than memory foam but offering consistent support. Its natural breathability keeps you cool.
- Pros:
- Durable, often lasting 12-15 years without sagging.
- Naturally cooling, ideal for inflammation-related heat sensitivity.
- Eco-friendly options (e.g., organic latex) appeal to health-conscious buyers.
- Cons:
- Higher cost, with quality latex mattresses starting at $1,500.
- Firmer feel may not suit those seeking deep cushioning.
- Heavier, making setup or rotation challenging.
- Best For: Back sleepers, eco-conscious individuals, or those needing firm, responsive support.
- Example: A 10-inch zoned latex mattress with a medium-firm feel and an organic cotton cover for breathability.
- Hybrid (Innerspring + Foam/Latex):
- How It Works: Pocketed coils provide robust support, while foam or latex layers add cushioning. This combination balances firmness and comfort, adapting to various sleep positions.
- Pros:
- Excellent airflow, reducing heat buildup.
- Strong edge support, aiding mobility.
- Versatile, suiting side, back, and combination sleepers.
- Cons:
- Quality varies widely; low-end hybrids may use thin foam layers.
- Less motion isolation than all-foam mattresses.
- May be noisier if coils are poorly constructed.
- Best For: Combination sleepers, heavier individuals, or those seeking a traditional “mattress feel” with modern upgrades.
- Example: A 12-inch hybrid with pocketed coils, a 2-inch latex comfort layer, and zoned lumbar support.
Research Insights:
- A 2015 study in Sleep Health found that hybrid mattresses improved sleep quality and reduced back pain in patients with chronic lumbar issues, thanks to their balanced support and pressure relief.
- A 2018 review in Journal of Chiropractic Medicine noted that medium-firm foam and latex mattresses alleviated pain in patients with disc-related conditions, with latex offering better durability.
LSI Keywords: Memory foam mattress, latex mattress, hybrid mattress, back pain relief, sciatica support, durable mattress.
Additional Factors to Enhance Sleep Quality
Beyond the mattress itself, several factors can optimize your sleep environment and support recovery from lumbar nerve root inflammation.
- Mattress Toppers:
- A 2-3 inch memory foam or latex topper can soften a slightly firm mattress or add pressure relief to an aging one. Ensure the topper is high-density to avoid premature wear.
- Toppers are a cost-effective alternative to replacing a mattress, but they can’t fix a severely sagging or unsupportive base.
- Adjustable Beds:
- Adjustable bases allow you to elevate your legs or head, reducing lumbar pressure and improving circulation. They’re particularly helpful for back sleepers with sciatica.
- Pair with a flexible mattress (foam or hybrid) to ensure compatibility.
- Trial Periods and Warranties:
- Opt for a 90-120 day trial to test the mattress’s impact on pain and sleep quality. Most reputable brands offer this, along with 10-20 year warranties covering sagging or defects.
- Sleep trials give you peace of mind, as adaptation to a new mattress can take 30-60 days.
- Body Weight Considerations:
- Heavier individuals (>200 lbs) need thicker mattresses (12-14 inches) with firmer support to prevent sinking, which can exacerbate nerve compression.
- Lighter individuals (<150 lbs) may find medium or medium-soft mattresses sufficient, as they exert less pressure on the mattress.
- Complementary Bedding:
- Use a medium-firm pillow to support neck alignment, preventing strain that could worsen back pain.
- A waterproof, breathable mattress protector extends mattress life and maintains hygiene.
- Consulting Healthcare Providers:
- Work with a doctor or physical therapist to ensure your mattress aligns with your treatment plan, which may include exercises to strengthen the core and improve spinal stability.
- A 2020 study in Spine Journal emphasized the role of sleep environment optimization in enhancing outcomes for disc herniation patients.
LSI Keywords: Adjustable bed, mattress topper, sleep trial, spinal support, back pain management.
Recommended Mattresses for Lumbar Disc Herniation
Based on the detailed analysis above, here are specific mattress recommendations tailored to different needs:
- Best Overall: A 12-inch medium-firm hybrid mattress with pocketed coils, a 2-inch natural latex comfort layer, and zoned lumbar support. Look for brands like Saatva or Helix, with strong trial periods and cooling features.
- Best for Side Sleepers: A 12-inch medium-firm memory foam mattress with gel-infused foam and a high-density base. Tempur-Pedic or Nectar models offer excellent pressure relief and motion isolation.
- Best for Back Sleepers: A 10-12 inch zoned latex mattress with a medium-firm feel and organic materials. Avocado or Birch mattresses provide durability and breathability.
- Best Budget Option: A 10-inch medium-firm memory foam mattress with a 100-night trial, such as those from Zinus or Tuft & Needle, ensuring affordability without sacrificing support.
- Best for Heavier Individuals: A 14-inch hybrid with reinforced coils and a thick foam layer, like the WinkBeds Plus, designed for durability and robust lumbar support.
Always verify firmness, trial periods, and return policies to ensure the mattress meets your needs.
FAQ: Addressing Common Concerns
Q: What firmness level is best for lumbar disc herniation and nerve inflammation?
A: A medium-firm mattress (5-7/10) strikes the ideal balance, supporting spinal alignment while cushioning pressure points. Research, like the 2003 Lancet study, supports this for back pain relief. Adjust based on body weight—slightly softer for lighter individuals, firmer for heavier ones.
Q: Can a mattress topper help if I’m not ready to buy a new mattress?
A: Absolutely. A 2-3 inch high-density memory foam or latex topper can enhance pressure relief and support, especially if your current mattress is slightly firm or aging. However, toppers can’t compensate for a severely worn or unsupportive mattress.
Q: How long does it take to adjust to a new mattress?
A: Expect 30-60 days to fully adapt, as your body adjusts to new support and firmness. Use the trial period (90-120 days) to assess pain relief, sleep quality, and comfort. Keep a sleep diary to track improvements.
Q: Are adjustable beds worth it for disc herniation?
A: Yes, adjustable beds allow you to elevate your legs or upper body, reducing lumbar pressure and easing sciatica symptoms. They’re most effective with foam or hybrid mattresses, which flex without losing support. Consult your doctor to ensure compatibility with your condition.
Q: How often should I replace my mattress to manage back pain?
A: Replace every 7-10 years, or sooner if you notice sagging, lumps, or increased pain. A worn mattress loses its ability to support spinal alignment, worsening nerve inflammation. Regular rotation (every 3-6 months) extends mattress life.
Q: Can a mattress alone resolve my back pain?
A: While a supportive mattress significantly reduces pain and improves sleep, it’s not a cure. Combine it with physical therapy, core-strengthening exercises, and medical guidance for comprehensive management. A 2021 study in Pain Medicine highlighted the synergy of sleep optimization and active treatment.
LSI Keywords: Mattress replacement, adjustable bed benefits, back pain solutions, sleep posture, sciatica mattress.
How to sleep with herniated disc l5-s1
Sleeping with a herniated disc at the L5-S1 level (the lowest lumbar vertebra and the first sacral segment) can be challenging due to pain, nerve irritation, and potential sciatica symptoms. The goal is to maintain spinal alignment, reduce pressure on the affected disc, and minimize nerve root irritation. Below is a detailed, medically-informed guide on how to sleep comfortably with an L5-S1 herniated disc, incorporating sleep positions, bedding adjustments, and practical tips to alleviate pain and promote restful sleep. The tone is compassionate and practical, with clear steps to help you find relief.
Understanding L5-S1 Herniated Disc and Its Impact on Sleep
The L5-S1 disc is located in the lower back, where the lumbar spine meets the sacrum. A herniation here can compress the L5 or S1 nerve roots, causing lower back pain, sciatica (radiating pain, numbness, or tingling down the leg), and muscle weakness. These symptoms often worsen at night due to prolonged positioning or improper spinal alignment, disrupting sleep and slowing recovery.
- Why Sleep Matters: Quality sleep reduces inflammation, supports tissue repair, and helps manage pain perception, all critical for healing a herniated disc.
- Challenges: Lying down can increase disc pressure or nerve irritation, especially in unsupportive positions or on an unsuitable mattress.
- Goal: Adopt sleep strategies that maintain the spine’s natural curves, decompress the L5-S1 region, and minimize nerve root irritation.
Best Sleep Positions for L5-S1 Herniated Disc
Choosing the right sleep position is crucial to reduce strain on the herniated disc and alleviate nerve compression. Below are the most effective positions, with tips to optimize comfort.
1. Side Sleeping in the Fetal Position
- Why It Helps: Sleeping on your side with your knees slightly bent toward your chest opens the spaces between vertebrae, reducing pressure on the L5-S1 disc and irritated nerve roots. This position is particularly effective for sciatica relief.
- How to Do It:
- Lie on your side (preferably the less painful side if sciatica is unilateral).
- Bend your knees to a comfortable angle, mimicking a gentle fetal curl.
- Place a firm pillow between your knees to align your hips and prevent your top leg from sliding forward, which could twist the lumbar spine.
- Use a medium-firm head pillow to keep your neck aligned with your spine, avoiding forward tilt.
- Tips:
- If sciatica affects one leg, try sleeping with the painful side up to reduce nerve compression.
- Avoid curling too tightly, as this can strain the lower back or restrict breathing.
- Why It Works: A 2017 study in Journal of Orthopedic Research noted that side sleeping with proper pelvic alignment reduces lumbar stress, beneficial for disc herniation patients.
2. Back Sleeping with Knee Support
- Why It Helps: Lying on your back with a pillow under your knees maintains the natural lumbar curve, reducing pressure on the L5-S1 disc and preventing nerve root irritation. This position evenly distributes body weight, minimizing pressure points.
- How to Do It:
- Lie flat on your back on a supportive mattress.
- Place a small pillow, rolled towel, or foam wedge under your knees to elevate them slightly (about 30-45 degrees).
- Optionally, place a thin towel roll under the small of your back for added lumbar support.
- Use a low-profile head pillow to keep your neck neutral, avoiding excessive forward tilt.
- Tips:
- Adjust the knee pillow height to avoid over-flexing the hips, which could strain the lower back.
- If you feel stiffness, try gentle stretches before bed to relax the lumbar muscles.
- Why It Works: A 2019 study in Spine Journal found that back sleeping with knee elevation reduces intradiscal pressure, easing symptoms of lumbar herniation.
3. Avoid Stomach Sleeping
- Why to Avoid: Sleeping on your stomach arches the lower back, increasing pressure on the L5-S1 disc and compressing nerve roots. It also forces the neck to twist, potentially causing additional strain.
- What to Do Instead: If you’re a stomach sleeper, transition to side or back sleeping gradually. Use body pillows to “hug” while side sleeping, mimicking the feel of stomach sleeping while protecting your spine.
- Tip: Place a pillow under your pelvis temporarily if you must sleep on your stomach, but aim to switch positions to prevent worsening symptoms.
Optimizing Your Sleep Environment
Beyond sleep position, your mattress, pillows, and bedding play a critical role in managing L5-S1 herniated disc pain. Here’s how to create a supportive sleep setup.
1. Choose a Supportive Mattress
- Ideal Firmness: A medium-firm mattress (5-7 on a 10-point scale) is best, as it supports spinal alignment without creating pressure points. A 2003 study in The Lancet found medium-firm mattresses reduce low back pain more effectively than very firm or soft ones.
- Recommended Types:
- Memory Foam: Contours to your body, relieving pressure on the hips and shoulders. Look for high-density foam (4-5 lbs/ft³) with gel infusion for cooling.
- Latex: Offers responsive support and durability, ideal for back sleepers. Natural latex is breathable, reducing heat buildup.
- Hybrid: Combines pocketed coils for support with foam or latex for cushioning, suitable for combination sleepers.
- Features to Prioritize:
- Zoned Support: Firmer foam or coils under the hips/lumbar region maintain spinal alignment.
- Pressure Relief: A 2-3 inch comfort layer cushions sensitive areas, reducing sciatica discomfort.
- Thickness: 10-12 inches for most; 12-14 inches for heavier individuals (>200 lbs).
- Trial Period: Choose a mattress with a 90-120 day trial to test its impact on pain relief, as adaptation can take 30-60 days.
2. Use Supportive Pillows
- Knee Pillow: For side sleepers, a firm pillow between the knees aligns the pelvis. For back sleepers, a pillow under the knees reduces lumbar strain.
- Lumbar Support: A small towel roll or lumbar pillow under the lower back while back sleeping enhances the natural curve.
- Head Pillow: A medium-firm, contoured cervical pillow keeps the neck aligned with the spine, preventing strain that could exacerbate back pain.
- Body Pillow: Hugging a body pillow while side sleeping stabilizes your position and mimics the comfort of stomach sleeping.
3. Consider an Adjustable Bed
- Benefits: Adjustable beds allow you to elevate your legs or upper body, reducing L5-S1 disc pressure and easing sciatica. A slight incline (zero-gravity position) can decompress the spine.
- Compatibility: Pair with a flexible mattress (memory foam or hybrid) to ensure smooth adjustment.
- Research: A 2020 study in Pain Medicine noted that adjustable beds improved sleep quality in patients with chronic back pain.
4. Add a Mattress Topper (If Needed)
- If your mattress is too firm or slightly worn, a 2-3 inch memory foam or latex topper can add pressure relief and support. Ensure the topper is high-density to avoid sagging.
- Note: Toppers can’t fix a severely unsupportive mattress, so replace it if it’s sagging or over 7-10 years old.
5. Maintain a Cool Sleep Environment
- Inflammation at L5-S1 can increase heat sensitivity. Choose a mattress with cooling features (gel foam, latex, or breathable hybrid) and use lightweight, breathable bedding (cotton or bamboo sheets).
- Keep your bedroom at 60-67°F (16-19°C) to promote restful sleep, as recommended by the National Sleep Foundation.
Practical Tips for Better Sleep with L5-S1 Herniated Disc
- Establish a Pre-Sleep Routine:
- Perform gentle stretches (e.g., cat-cow, knee-to-chest) 10-15 minutes before bed to relax lumbar muscles and improve flexibility. Consult a physical therapist for tailored exercises.
- Apply a warm compress to the lower back for 15 minutes to reduce muscle tension, followed by a cool pack if inflammation is acute.
- Manage Pain Before Bed:
- Take prescribed anti-inflammatory medications or muscle relaxants as directed by your doctor, timed to cover the night.
- Avoid heavy meals, caffeine, or alcohol 2-3 hours before bed, as they can disrupt sleep or increase inflammation.
- Practice Position Transitions:
- If you shift positions during sleep, move slowly to avoid jarring the spine. Use your arms to support your weight when rolling from back to side.
- Place a pillow strategically to “guide” you into a supportive position if you tend to revert to stomach sleeping.
- Monitor Sleep Quality:
- Keep a sleep diary to track pain levels, sleep duration, and position effectiveness. Share this with your doctor to refine your strategy.
- If pain consistently wakes you, consult your healthcare provider to assess if imaging (e.g., MRI) or treatments (e.g., epidural injections) are needed.
- Work with Healthcare Professionals:
- A physical therapist can recommend specific sleep postures and exercises to strengthen core muscles, stabilizing the L5-S1 region.
- A doctor may suggest complementary treatments like acupuncture or chiropractic care, but ensure they’re evidence-based and tailored to your condition.
Soft or Firm Mattress For Herniated Disc
For a herniated disc, particularly at the L5-S1 level, a medium-firm mattress (5-7 on a 10-point firmness scale) is generally recommended over a very soft or very firm mattress. Here’s a concise explanation of why, tailored to your needs, with evidence-based insights and practical considerations.
Why Medium-Firm is Best for a Herniated Disc
- Spinal Alignment: A medium-firm mattress supports the natural curves of your spine (cervical, thoracic, lumbar) without allowing the hips to sink too deeply (as with soft mattresses) or creating excessive pressure points (as with very firm mattresses). Proper alignment reduces strain on the L5-S1 disc and irritated nerve roots.
- Pressure Relief: It provides enough cushioning to relieve pressure on the hips and shoulders, especially for side sleepers, while maintaining support to prevent nerve compression.
- Research Support: A 2003 study in The Lancet found that medium-firm mattresses significantly reduced low back pain compared to very firm or soft ones in patients with chronic lumbar issues, including disc herniation.
- Adaptability: Medium-firm mattresses suit both side sleeping (fetal position) and back sleeping (with a pillow under the knees), the two best positions for L5-S1 herniated disc pain relief.
Why Avoid Very Soft Mattresses
- Problem: Soft mattresses (<4/10 firmness) allow the hips and pelvis to sink excessively, curving the lumbar spine and increasing pressure on the herniated disc. This can worsen nerve root irritation and sciatica.
- Impact: You may wake up with increased pain or stiffness, as the spine is misaligned for hours.
- Exception: Very soft mattresses might feel comfortable initially for lightweight individuals (<150 lbs), but they often fail to provide long-term support for disc issues.
Why Avoid Very Firm Mattresses
- Problem: Very firm mattresses (>8/10 firmness) lack contouring, creating pressure points at the hips, shoulders, and lower back. This can exacerbate pain, especially for side sleepers, and fail to cushion inflamed areas.
- Impact: They may feel supportive but can increase discomfort by not adapting to the body’s natural shape, potentially worsening nerve irritation.
- Exception: Heavier individuals (>200 lbs) may tolerate slightly firmer mattresses (closer to 7/10) to prevent sinking, but extreme firmness is still suboptimal.
Key Considerations
- Body Weight:
- Lighter Individuals (<150 lbs): A medium-firm mattress leaning slightly softer (5-6/10) may suffice, as they exert less pressure on the mattress.
- Heavier Individuals (>200 lbs): A medium-firm mattress leaning firmer (6-7/10) ensures adequate support to prevent sinking, which could stress the L5-S1 disc.
- Sleep Position:
- Side Sleepers: Need medium-firm with a 2-3 inch comfort layer (memory foam or latex) for hip/shoulder cushioning.
- Back Sleepers: Benefit from medium-firm with zoned lumbar support to maintain the spine’s natural curve.
- Mattress Type:
- Memory Foam: High-density (4-5 lbs/ft³), medium-firm options contour well and relieve pressure (e.g., Tempur-Pedic).
- Latex: Naturally medium-firm and responsive, ideal for durability and cooling (e.g., Avocado).
- Hybrid: Combines coils and foam/latex for balanced support and breathability (e.g., Saatva).
- Trial Period: Choose a mattress with a 90-120 day trial to test its impact on pain, as adaptation can take 30-60 days.
Practical Recommendations
- Best Choice: A medium-firm mattress (5-7/10) with zoned support (firmer under the hips/lumbar region) and a pressure-relieving comfort layer (2-3 inches of memory foam or latex). Examples include:
- Memory Foam: Nectar Premier (medium-firm, gel-infused for cooling).
- Latex: Birch Natural Mattress (medium-firm, breathable).
- Hybrid: Helix Midnight (medium-firm, zoned coils).
- Topper Option: If replacing your mattress isn’t feasible, add a 2-3 inch medium-firm memory foam or latex topper to a slightly firm base mattress for better contouring, but ensure the base isn’t sagging.
- Test and Adjust: Use the trial period to assess pain relief. Pair with proper sleep posture (side with knee pillow, back with knee support) to maximize benefits.
Final Note
A medium-firm mattress is the Goldilocks solution for an L5-S1 herniated disc, balancing support and comfort to reduce pain and promote healing. Avoid very soft mattresses that misalign the spine or very firm ones that create pressure points. Consult your doctor or physical therapist to ensure your mattress choice complements your treatment plan, and consider your body weight and sleep position when selecting firmness. With the right mattress, you can sleep more comfortably and support your recovery.
Disclaimer: This advice is general and not a substitute for medical guidance. If pain, numbness, or weakness worsens, seek professional medical evaluation.
Can a Bad Mattress Cause a Herniated Disc
While a bad mattress may not directly cause a herniated disc, it can significantly worsen symptoms of an existing L5-S1 herniation by:
- Increasing Nerve Irritation: A sagging mattress may exacerbate sciatica by compressing nerve roots further, as the spine is misaligned.
- Amplifying Pain: Pressure points from a too-firm mattress or uneven support from a worn-out one can heighten lower back and leg pain, disrupting sleep.
- Slowing Healing: Poor sleep quality due to discomfort reduces the body’s ability to reduce inflammation and repair disc tissue, prolonging recovery. A 2020 study in Pain Medicine emphasized the role of sleep quality in managing chronic back pain.
- Encouraging Poor Sleep Posture: A bad mattress may force you into unsupportive positions (e.g., stomach sleeping), increasing disc pressure and nerve compression.
What Defines a “Bad” Mattress?
A mattress is considered “bad” for spinal health if it:
- Sags or Has Lumps: Indentations or uneven surfaces disrupt spinal alignment.
- Is Too Soft (<4/10): Allows excessive sinking, misaligning the lumbar spine.
- Is Too Firm (>8/10): Creates pressure points and fails to contour to the body.
- Lacks Support: Fails to maintain the spine’s natural “S” curve or distribute weight evenly.
- Is Old (>7-10 Years): Worn-out materials lose their ability to provide support, even if the mattress was initially suitable.
What Mattress is Best to Prevent or Manage Herniated Disc Issues?
To minimize the risk of disc strain and support an existing L5-S1 herniated disc, choose a medium-firm mattress (5-7/10 firmness). Here’s why it’s ideal and how to select one:
- Why Medium-Firm:
- Balances support and cushioning, maintaining spinal alignment while relieving pressure on hips and shoulders.
- Reduces intradiscal pressure and nerve irritation, as supported by a 2003 Lancet study showing medium-firm mattresses improve low back pain outcomes.
- Suits recommended sleep positions: side (fetal with knee pillow) and back (with knee support).
- Recommended Features:
- Zoned Support: Firmer foam/coils under the hips/lumbar region to support the L5-S1 area.
- Pressure Relief: 2-3 inch comfort layer (memory foam or latex) to cushion pressure points.
- Materials:
- Memory Foam: High-density (4-5 lbs/ft³), medium-firm for contouring (e.g., Tempur-Pedic).
- Latex: Naturally medium-firm, durable, and cooling (e.g., Avocado).
- Hybrid: Pocketed coils with foam/latex for support and breathability (e.g., Saatva).
- Thickness: 10-12 inches for most; 12-14 inches for heavier individuals (>200 lbs).
- Body Weight Considerations:
- Lighter (<150 lbs): Medium-firm leaning softer (5-6/10) for adequate cushioning.
- Heavier (>200 lbs): Medium-firm leaning firmer (6-7/10) to prevent sinking.
- Trial Period: Opt for a 90-120 day trial to test pain relief, as adaptation takes 30-60 days.
Practical Steps to Protect Your Spine
While a bad mattress may contribute to disc stress, a good mattress and sleep habits can support spinal health and manage herniated disc symptoms:
- Replace an Old Mattress: If your mattress is sagging or over 7-10 years old, replace it with a medium-firm model to reduce spinal strain.
- Use a Topper Temporarily: A 2-3 inch medium-firm memory foam or latex topper can improve a slightly unsupportive mattress, but replace a severely worn one.
- Adopt Proper Sleep Posture:
- Side (Fetal): Pillow between knees to align hips.
- Back: Pillow under knees to maintain lumbar curve.
- Avoid Stomach Sleeping: Increases L5-S1 disc pressure.
- Complement with Lifestyle Changes:
- Maintain a healthy weight to reduce disc stress.
- Practice good posture during the day to avoid cumulative strain.
- Engage in core-strengthening exercises (guided by a physical therapist) to stabilize the spine.
- Consult a Doctor: If you suspect a herniated disc or experience worsening pain, numbness, or weakness, seek medical evaluation. Imaging (e.g., MRI) and treatments like physical therapy or injections may be needed.
Best mattress for L5-S1 herniated disc
For an L5-S1 herniated disc, the best mattress is medium-firm (5-7/10) to support spinal alignment, reduce pressure on the disc, and relieve sciatica. Key features include zoned support (firmer under hips/lumbar), pressure-relieving materials (memory foam, latex, or hybrid), and a 10-12 inch thickness (12-14 for heavier individuals).
Top picks: Saatva Classic (hybrid) for overall support, Tempur-Pedic TEMPUR-Adapt (memory foam) for side sleepers, Avocado Green (latex) for back sleepers, and Nectar Premier (memory foam) for budget buyers. Pair with side (fetal) or back (knee pillow) sleeping, and use a 90-120 day trial to test pain relief. Consult a doctor to align with your treatment plan.
How to sleep with degenerative disc disease in lower back
Sleeping with degenerative disc disease (DDD) in the lower back, particularly affecting the L5-S1 region, can be challenging due to pain, stiffness, and potential nerve irritation. DDD involves the gradual breakdown of spinal discs, leading to reduced cushioning, inflammation, and sometimes herniation or nerve compression (e.g., sciatica). The goal is to adopt sleep strategies that maintain spinal alignment, minimize pressure on the affected discs, and promote restorative rest. Below is a concise, medically-informed guide on how to sleep comfortably with lower back DDD, focusing on sleep positions, mattress choices, bedding adjustments, and practical tips. This response complements your interest in mattresses for L5-S1 herniated discs, ensuring a tailored approach for DDD.
Best Sleep Positions for Lower Back DDD
Proper sleep posture reduces strain on degenerated discs and alleviates nerve irritation. Here are the most effective positions:
- Side Sleeping (Fetal Position)
- Why It Helps: Sleeping on your side with knees slightly bent opens the spaces between vertebrae, reducing pressure on lower back discs and nerves. This is ideal for sciatica relief.
- How to Do It:
- Lie on your side (preferably the less painful side if sciatica is present).
- Bend your knees to a gentle fetal curl (avoid over-curling to prevent strain).
- Place a firm pillow between your knees to align hips and prevent spinal twisting.
- Use a medium-firm head pillow to keep your neck aligned with your spine.
- Tip: If sciatica affects one leg, sleep with the painful side up to reduce nerve compression.
- Back Sleeping with Knee Support
- Why It Helps: Lying on your back with a pillow under your knees maintains the natural lumbar curve, distributing weight evenly and reducing disc pressure.
- How to Do It:
- Lie flat on a supportive mattress.
- Place a small pillow, rolled towel, or foam wedge under your knees (elevated ~30-45 degrees).
- Optionally, use a thin towel roll under the lower back for added lumbar support.
- Choose a low-profile head pillow to avoid neck strain.
- Tip: Adjust knee pillow height to avoid over-flexing hips, which could stress the lower back.
- Avoid Stomach Sleeping
- Why to Avoid: Stomach sleeping arches the lower back, increasing pressure on degenerated discs and irritating nerves. It also strains the neck.
- Alternative: If you prefer this position, transition to side or back sleeping using a body pillow to “hug” for comfort while maintaining spinal alignment.
Research Insight: A 2019 study in Spine Journal found that side and back sleeping with proper support reduce intradiscal pressure, easing symptoms of lumbar DDD.
Optimizing Your Sleep Environment
A supportive sleep setup enhances comfort and minimizes pain from DDD. Here’s how to optimize your mattress and bedding:
- Choose a Medium-Firm Mattress (5-7/10)
- Why It’s Best: A medium-firm mattress supports spinal alignment, cushions pressure points, and prevents the hips from sinking, which could stress degenerated discs. A 2003 Lancet study confirmed medium-firm mattresses reduce low back pain effectively.
- Recommended Types:
- Memory Foam: High-density (4-5 lbs/ft³), medium-firm, contours to the body (e.g., Tempur-Pedic TEMPUR-Adapt).
- Latex: Responsive, durable, and cooling, ideal for back sleepers (e.g., Avocado Green).
- Hybrid: Pocketed coils with foam/latex for support and breathability (e.g., Saatva Classic).
- Features:
- Zoned Support: Firmer under hips/lumbar to support the L5-S1 region.
- Pressure Relief: 2-3 inch comfort layer to cushion hips/shoulders.
- Thickness: 10-12 inches (12-14 for heavier individuals >200 lbs).
- Trial Period: Opt for a 90-120 day trial to test pain relief, as adaptation takes 30-60 days.
- Use Supportive Pillows
- Knee Pillow: For side sleepers, a firm pillow between the knees aligns the pelvis. For back sleepers, a pillow under the knees reduces lumbar strain.
- Lumbar Support: A small towel roll or lumbar pillow under the lower back while back sleeping enhances the natural curve.
- Head Pillow: A medium-firm, contoured cervical pillow keeps the neck aligned, preventing strain that could worsen back pain.
- Body Pillow: Hugging a body pillow while side sleeping stabilizes your position and eases the transition from stomach sleeping.
- Consider an Adjustable Bed
- Benefits: Elevating your legs or upper body (zero-gravity position) decompresses the lower back, reducing disc pressure and sciatica. A 2020 Pain Medicine study supports adjustable beds for back pain relief.
- Compatibility: Pair with a flexible mattress (memory foam or hybrid).
- Add a Mattress Topper (If Needed)
- A 2-3 inch medium-firm memory foam or latex topper can enhance a slightly firm or aging mattress, but replace a sagging or >7-10 year old mattress for best results.
- Keep It Cool
- DDD-related inflammation can increase heat sensitivity. Choose a cooling mattress (gel-infused foam, latex, or hybrid) and breathable bedding (cotton/bamboo). Maintain a bedroom temperature of 60-67°F, per the National Sleep Foundation.
Practical Tips for Better Sleep with DDD
- Pre-Sleep Routine:
- Do gentle stretches (e.g., knee-to-chest, pelvic tilts) for 10-15 minutes to relax lumbar muscles. Consult a physical therapist for tailored exercises.
- Apply a warm compress to the lower back for 15 minutes to ease tension, or a cool pack for acute inflammation.
- Pain Management:
- Take prescribed anti-inflammatory medications or muscle relaxants as directed, timed to cover the night.
- Avoid caffeine, heavy meals, or alcohol 2-3 hours before bed to reduce inflammation and sleep disruption.
- Position Transitions:
- Move slowly when shifting positions to avoid jarring the spine. Use your arms to support your weight when rolling.
- Place pillows strategically to guide you into supportive positions if you shift unconsciously.
- Monitor Symptoms:
- Keep a sleep diary to track pain, sleep quality, and position effectiveness. Share with your doctor to refine your approach.
- If pain, numbness, or weakness worsens, seek medical evaluation for imaging (e.g., MRI) or treatments like physical therapy or injections.
- Work with Professionals:
- A physical therapist can recommend core-strengthening exercises to stabilize the spine.
- A doctor may suggest complementary therapies (e.g., acupuncture) or assess for advanced interventions if conservative measures fail.
Summary
To sleep with lower back degenerative disc disease:
- Positions: Sleep on your side (fetal, with a knee pillow) or back (with a pillow under knees). Avoid stomach sleeping.
- Mattress: Choose a medium-firm (5-7/10) memory foam, latex, or hybrid mattress with zoned support and pressure relief (e.g., Saatva Classic, Tempur-Pedic TEMPUR-Adapt, Avocado Green).
- Bedding: Use knee, lumbar, and cervical pillows; consider an adjustable bed or topper.
- Tips: Stretch before bed, manage pain, keep the bedroom cool, and consult a doctor/physical therapist for a tailored plan.
Disclaimer: This is general advice and not a substitute for medical guidance. Seek professional evaluation for persistent or severe symptoms.
Conclusion
Lumbar spinal nerve root inflammation from disc herniation can make restful sleep feel elusive, but the right mattress can transform your nights and support your recovery. A medium-firm mattress with zoned support, high-quality materials like memory foam or latex, and excellent pressure relief aligns your spine, eases nerve pressure, and promotes healing.
Whether you choose a contouring memory foam, a responsive latex, or a versatile hybrid, prioritize features like cooling technology, strong edge support, and a generous trial period. By pairing your mattress with proper sleep posture and complementary bedding, you create a sleep environment that nurtures spinal health and reduces pain.
Always consult your healthcare provider to ensure your mattress choice aligns with your treatment plan, and take the time to test your new mattress thoroughly. With the right support beneath you, restful nights and brighter days are within reach.